Specimen quality
Mariana Berho
The pathologist is a key team-member in the treatment of patients with rectal cancer. Macroscopic benchmark quality indicators of treatment exist that surgeons should be aware of in the management of their patients.

Completeness of mesorectal excision
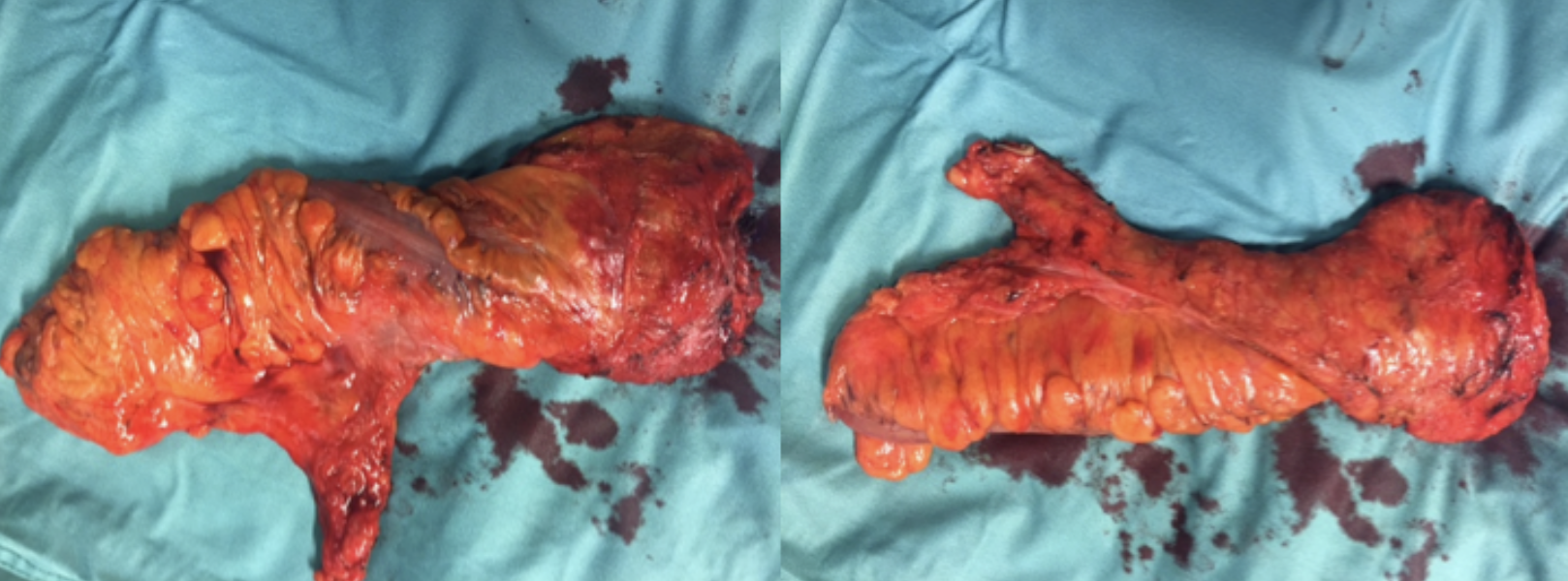
The surgical specimen is usually assessed immediately after surgery for an assessment of mesorectal quality at which point photographs are usually taken.The pathologist’s feedback can often advise the surgeon about areas where the procedure may have resulted in an oncologically inadequate specimen, thereby assisting the surgeon in improving his/her technique.
The completeness of a mesorectal excision is one of the main quality indicators of a rectal cancer procedure essentially ensuring that the rectum and mesorectal envelope are resected completely with data supporting higher local recurrence rates in patients with incomplete mesorectal excisions. (1)
The transanal total mesorectal excision has been proposed to potentially result in improved rates of mesorectal completeness given the improved visualization of the various peri-mesorectal planes, especially in the distal pelvis.
Example of TaTME-specimen after Cecil approach

Example of emptiness of pelvis after TaTME-procedure

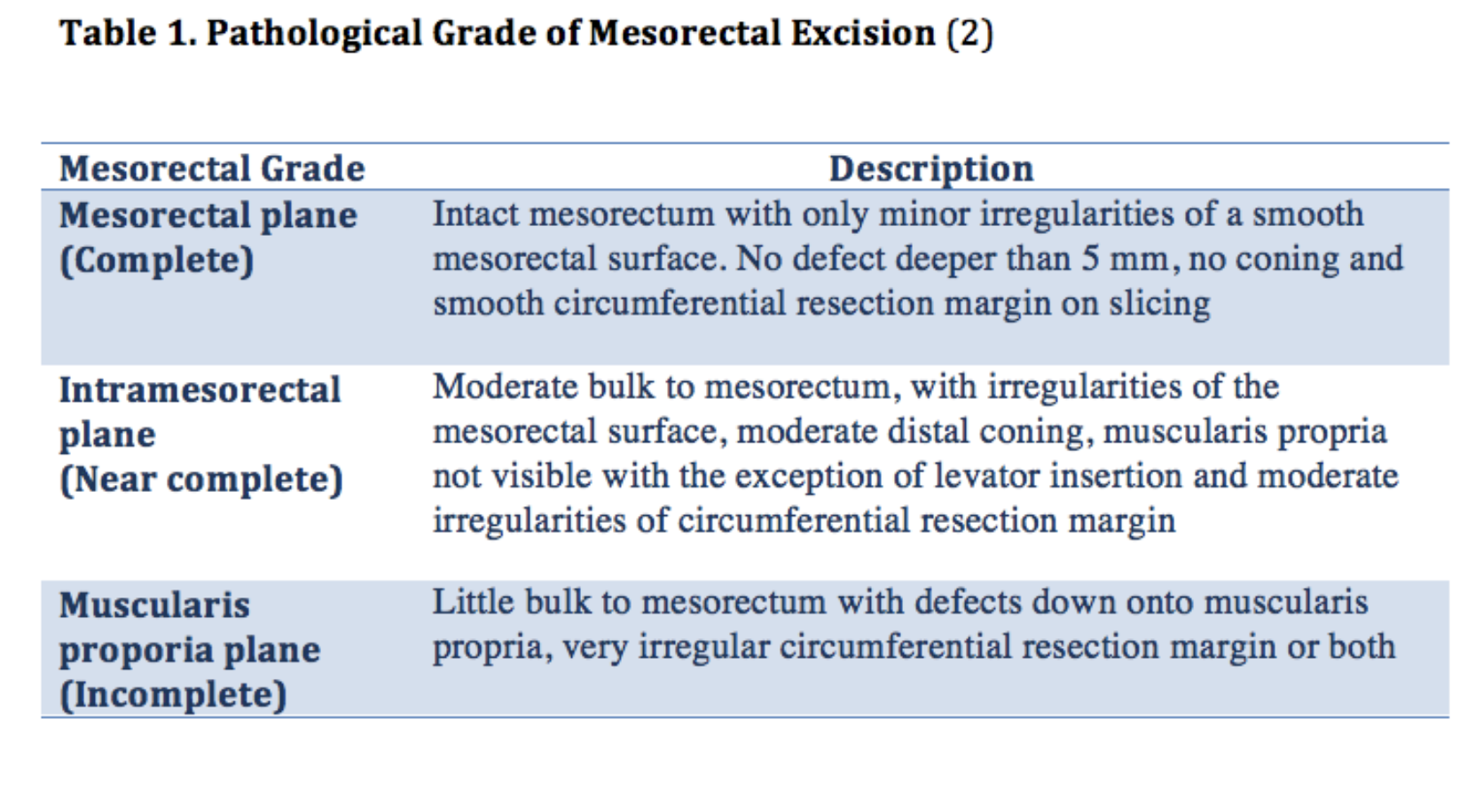
The currently accepted grading of mesorectal completeness was devised by Quirke and is described in Table 1. (2)
Circumferential resection margin
The circumferential resection margin informs the surgeon about the margin of adventitial soft tissue at the deepest post of the tumor’s invasion.
Previous studies have demonstrated this margin to represent the most important predictive factor for the outcome of local recurrence. (3)
After the specimen has been fixed in 10% formalin and the mesorectum has been painted with black ink, the pathologist performs transversal seriated sections (breadloafing) that will include representative areas of the tumor and mesorectum for eventual microscopic analysis.
The circumferential margin is often regarded as involved when the distance of malignant cells and the margin is ≤ 1mm. It should be noted that this involvement can result from malignant cells from the primary tumor or from a lymph node in proximity to the mesorectal plane of dissection.
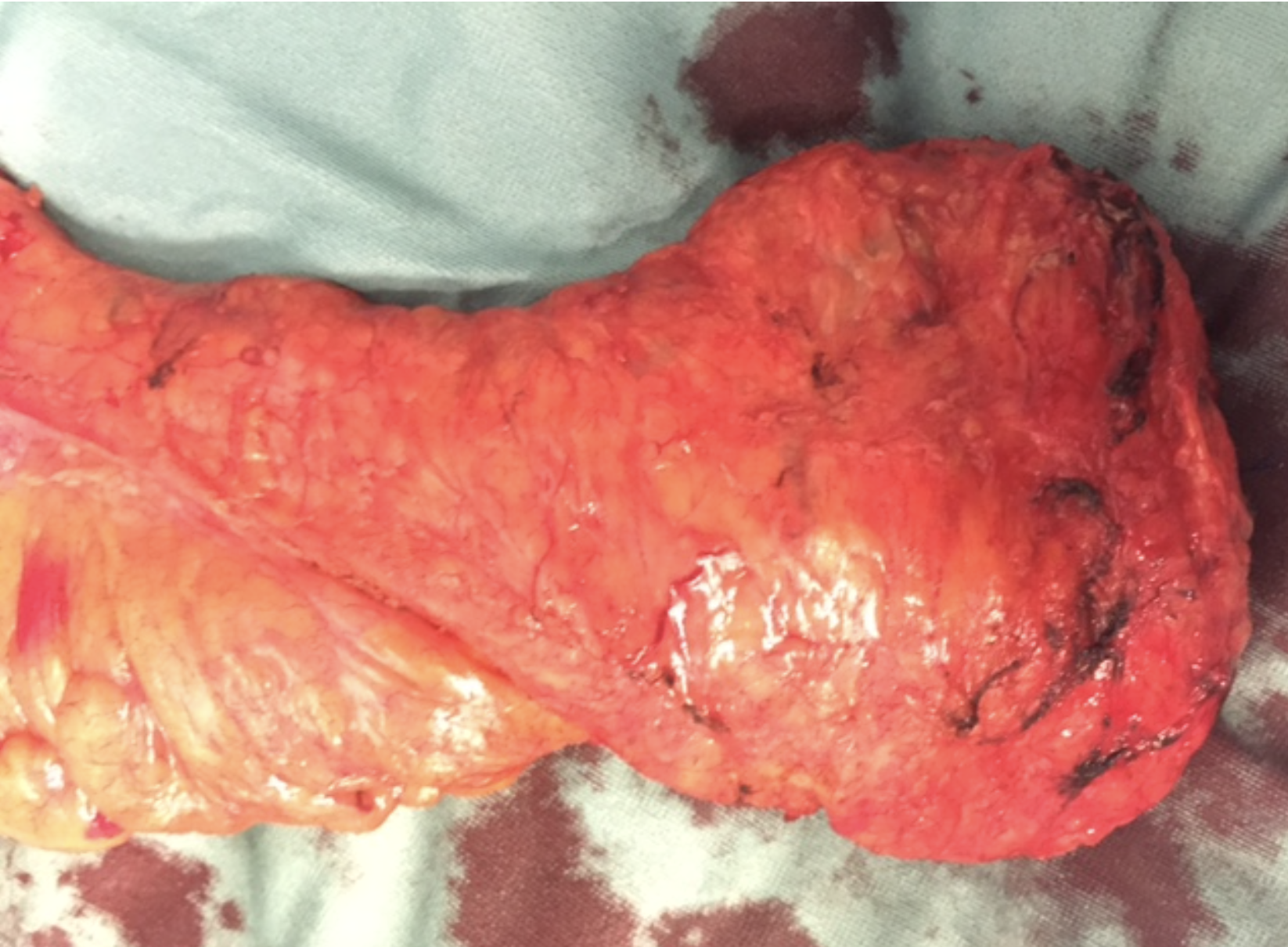
Intersphincteric resection
An intersphinteric dissection is more challenging than a regular low rectal dissection especially from a technical point of few. The risk of getting into the wrong plane is higher and a stepwise approach is crucial recognizing anatomical landmarks. Also specimen evaluation should be performed in a standardized way.
Next video shows a TaTME-procedure after an intersphincteric start during a live-surgery session in Berlin (06-2016). Discussion is focusing on planes of surgery and difficulty of performing a perimesorectal dissection after an intersphincteric start.
After the intersphincteric dissection the quality of the specimen is discussed by Mariana Berho (Cleveland Clinic), mainly focusing on completeness of the mesorectal excision, CRM and specimen handling.

References
1. Maslekar S, Sharma A, MacDonald A, Gunn J, Monson JRT, Hartley JE. Mesorectal grades predict recurrences after curative resection for rectal cancer. Diseases of the Colon & Rectum. 2007 Feb; 50(2): 168-75.
2. Quirke P. Training andquality assurance for rectal cancer: 20 years of data is enough. Lancet Oncology. 2003 Nov;4(11):695–702.
3. Quirke P, Durdey P, Dixon MF, Williams NS. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. The Lancet. 1986 Nov 1;2(8514):996–9.