Specimen extraction and reanastomosis
Mathieu D’Hondt
Mohammed Abu Hilal
After the TaTME procedure,specimen extraction and reanastomosis are important steps.
Specimen extraction
After completing the peri-mesorectal dissection from above and below, the TME-specimen is freed up and can be extracted either transabdominal or transanal.
Important: For all extraction sites a wound protector should be used to avoid tumor implants.
The choice where to extract the specimen depends mainly on the preference of the surgeon although some general rules can be taken into account.
Transanal specimen extraction
A transanal specimen extraction is only feasible when the bulk of mesorectum is limited and the anal canal is wide enough after removing the flexible platform. Before extraction the Inferior Mesenteric Artery (IMA) must be ligated by the abdominal team and most surgeons also divide the mesentery of the descending colon.
If a transanal extraction necessitates a functionally inferior straight anastomosis while transabdominal extraction allows a side-to-end anastomosis or J-pouch creation, we think it should be avoided.
The Alexis wound protector of Applied Medical can be used as a transanal extracton port although it wasn’t designed for that reason.
When performing transanal extraction it’s better to prepare the rectal pursestring upfront.
Transabdominal specimen extraction
When a transabdominal extraction is preferred, either a Pfannensteil incision or incison in the left or right iliac fossa can be used. The abdominal extraction port can also serve as the site for a diverting ileostomy although this might lead to a higher rate of parastomal hernias.
The anastomosis
Because the transanal portion of a TaTME-procedure starts with a rectotomy the technique always leaves an open distal rectal stump to be closed for reanastomosis.
Depending on the length of descending colon and the available space in the deep pelvis, one can choose a straight anastomosis (end-to-end), colonic J-pouch, or side-to-end anastomosis. For functional reasons a straight anastomosis should be avoided if possible.
The formation of a colorectal or coloanal anastomosis can be performed either by hand-sewn or stapling techniques.
When the TaTME procedure can be started with the platform in place, a higher length of rectal cuff usually remains and a stapled anastomosis can be achieved in most cases. This, of course, depends mostly on the height of the tumor and the requirement for adequate distal margins.
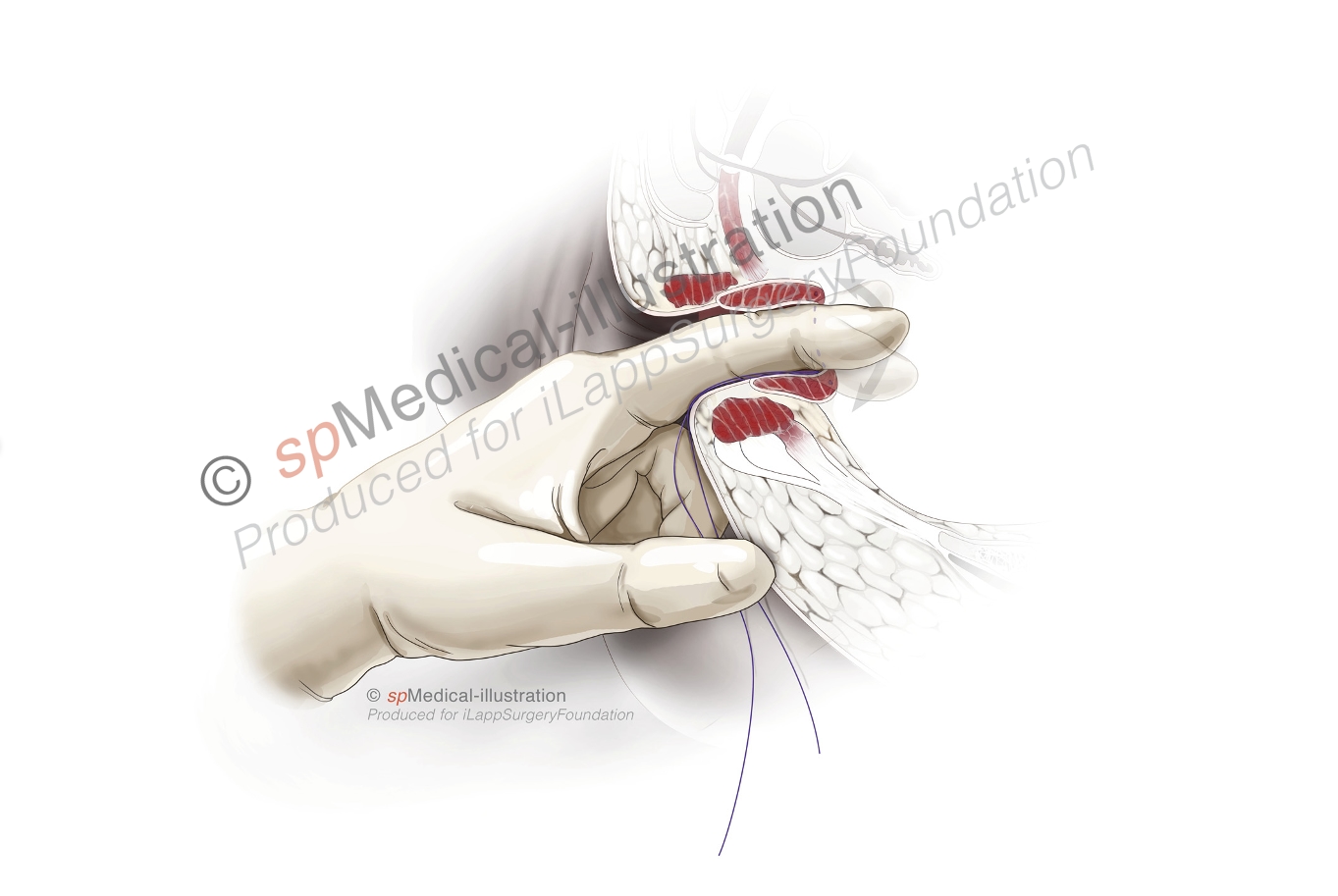
The quality of the anastomosis depends on a full thickness pursestring on the open rectal stump. This pursestring suture can be performed either through the flexible platform or after removing it, using a retractor if necessary. The tension on the elastic bands of the lonestar retractor can be adjusted to aid in getting better exposure. A 2-0 polypropylene suture is preferred in most patients.
The following components contribute to obtaining an optimal pursestring:
- full thickness bites but without imbricating too much rectal wall in each bite
- avoidance of gaps in the pursestring
- avoidance of imbricating the posterior wall of the vagina
- avoidance of imbricating sphincter muscle
- the first and last stitch should overlap
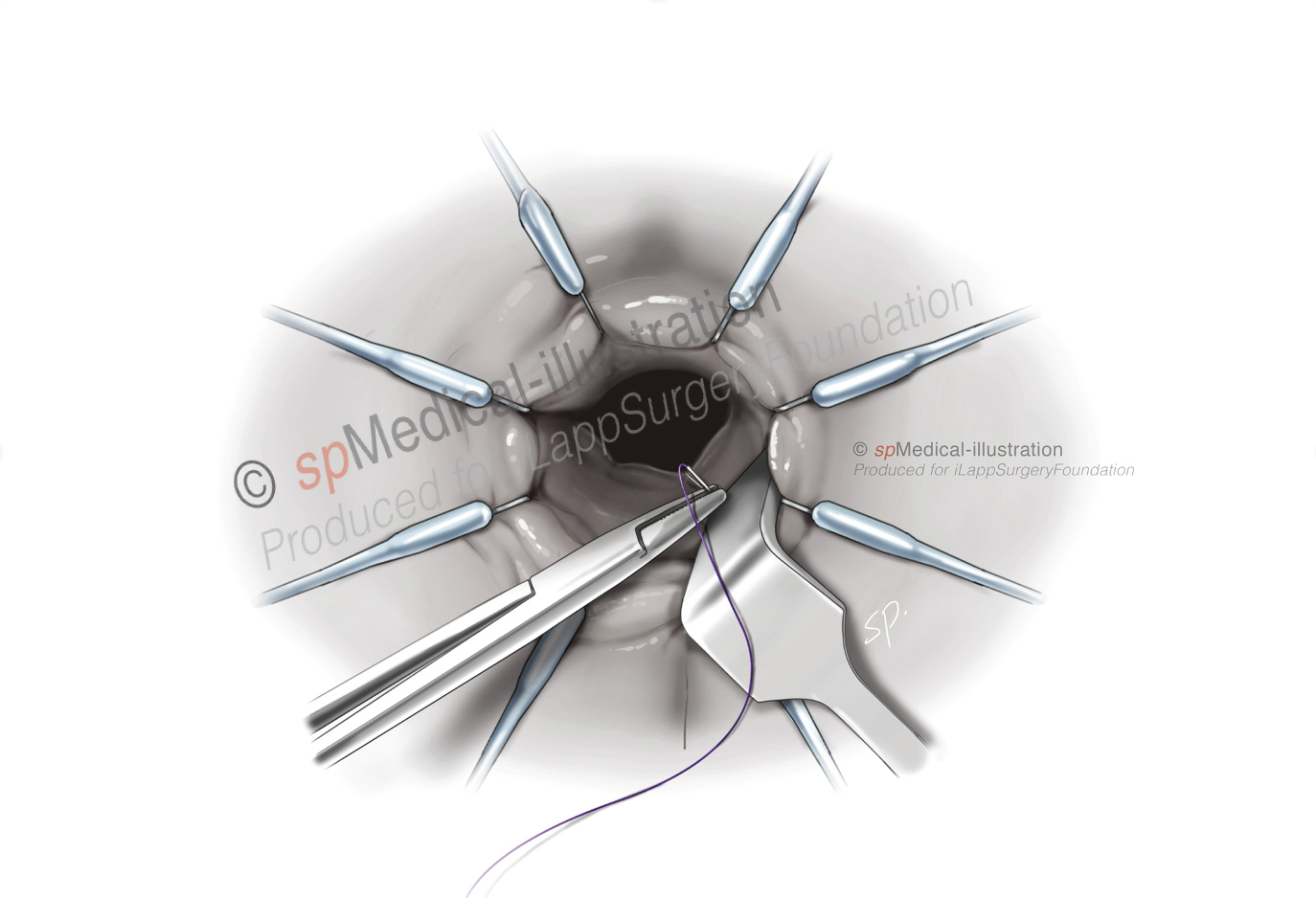
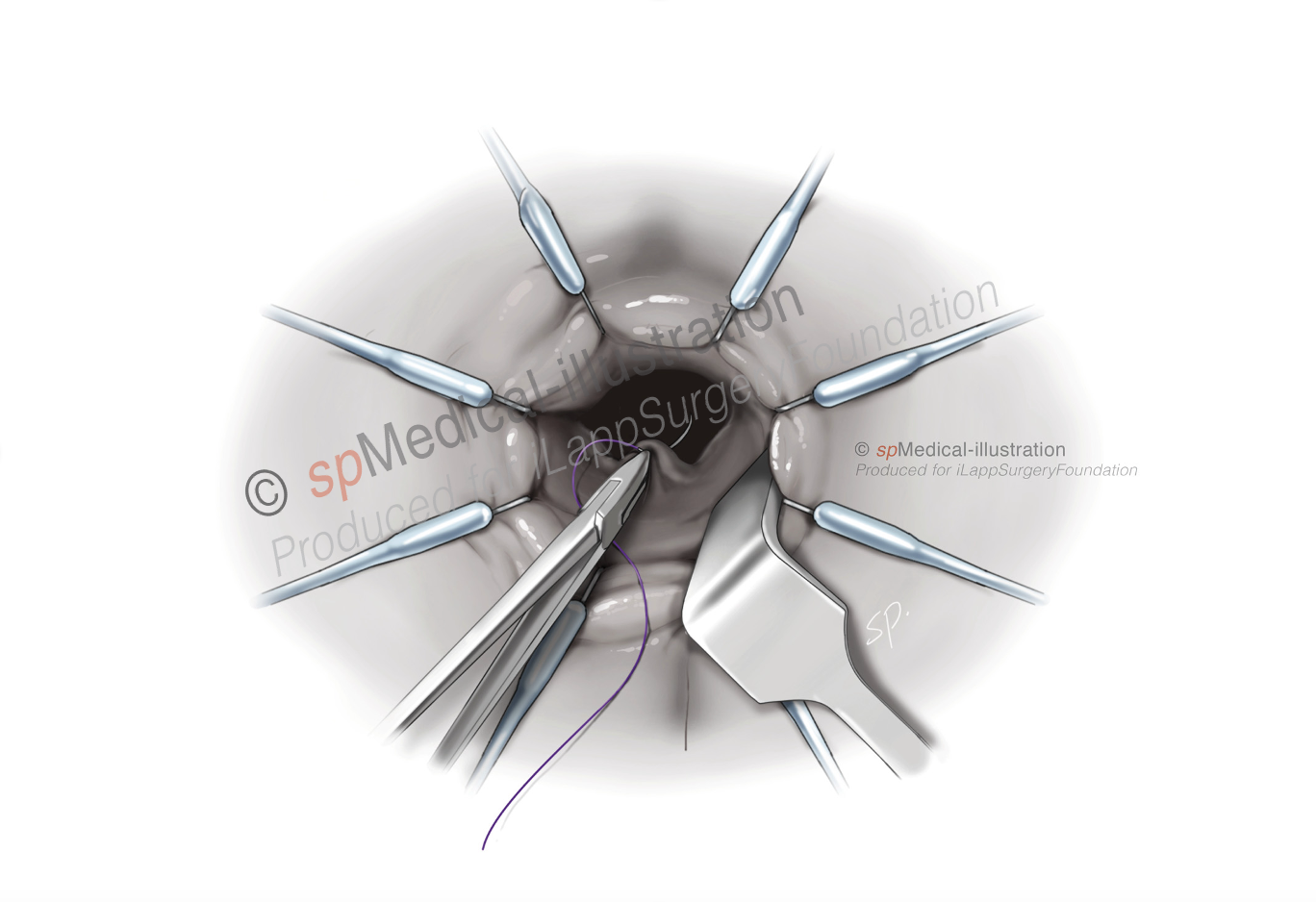

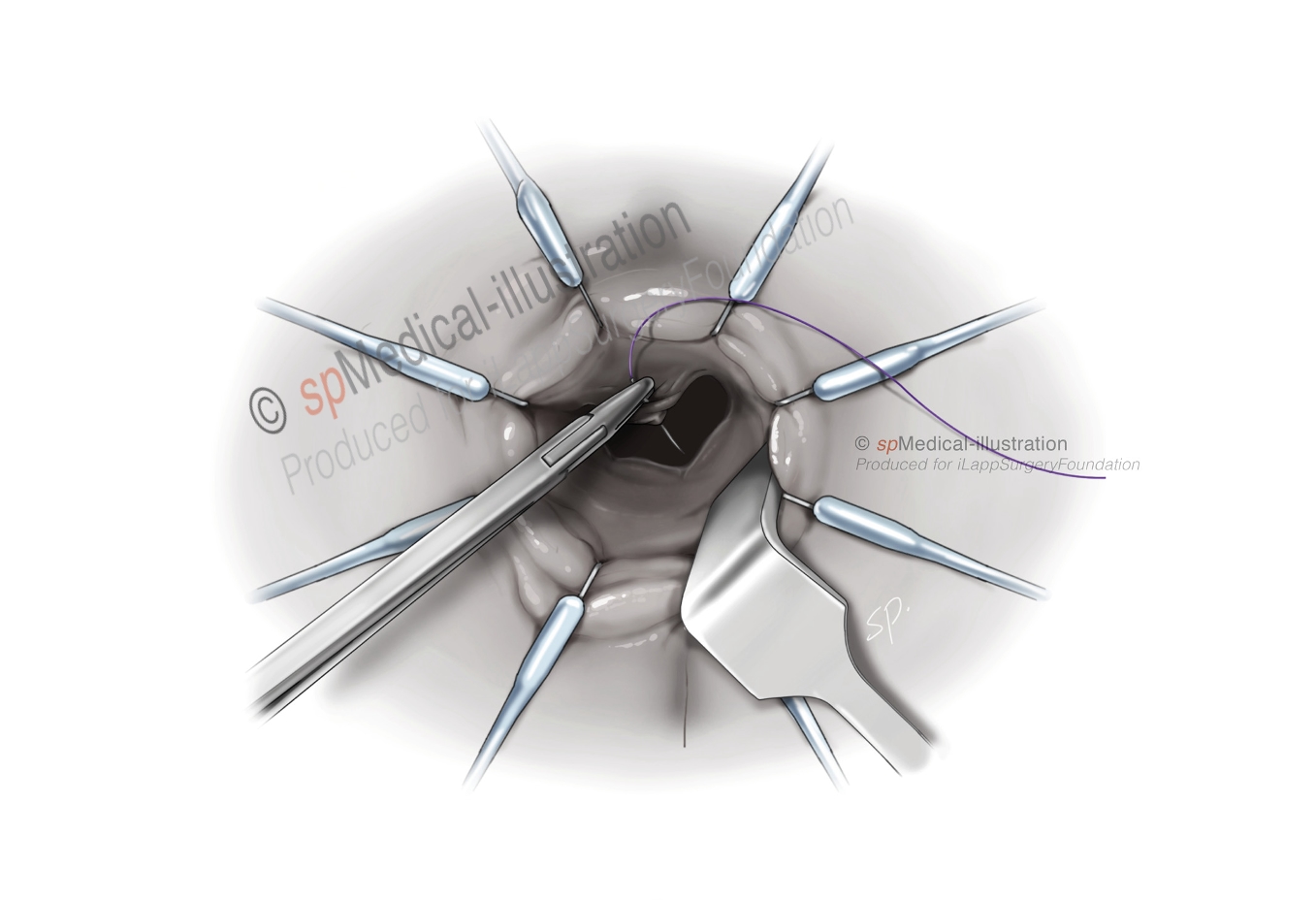

After the pursestring is performed the surgeon can introduce his/her index finger through it and free up the last bit of rectal cuff from surrounding tissues.
To guide the proximal colon towards the rectal stump several techniques can be used. Most often used are either an EEA haemorrhoid stapler or a modified technique using a 28-31 mm circular stapler.
EEA haemorrhoid stapled anastomosis
The anvil is secured in the proximal bowel using a 2-0 Prolene purse string suture. With the descending colon extruding through the anal canal, the surgeon seated at the perineum can perform this pursestring while afterwards also facilitating the creation of the pneumoperitoneum by pulling on it. By attaching a small piece of redivac drain to the anvil shaft it’s easier to grab it with a clamp introduced through the rectal stump.

The long anvil shaft (13.5 cm.) of the 33-mm EEA stapler (Medtronic) facilitates its passage through the anal canal to connect with the stapler device. After it is connected, the rectal cuff pursestring is tied to create the distal donut.
Firing of the stapler results in a “double pursestring – single stapled reanastomosis”. The 33 heamorrhoid stapler comes with a transparent proctoscope which can be used to check the completeness of the anastomosis. If necessary additional stitches can be placed to reinforce the suture line.

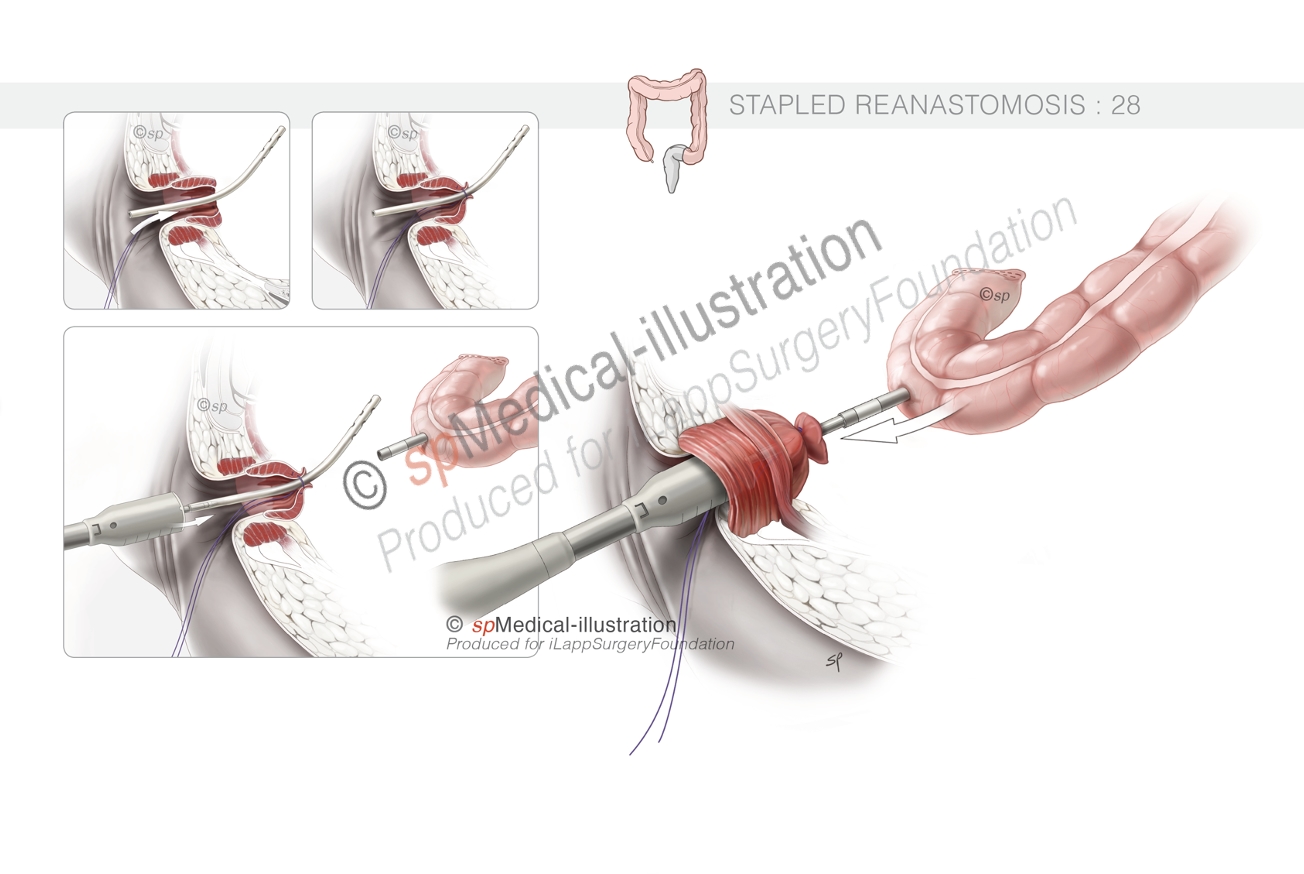
Modified circular stapled anastomosis, 28-31 mm
The anvil is tied into the proximal bowel using a 2-0 Prolene purse string suture. The spindle of a standard 28- or 31-mm stapler has a central opening.
A 10 Fr redivac drain is inserted through the central opening of the distal/rectal pursestring and held in place while tying. The spindle is then attached to the distal end of the drain and advanced into the pelvis. The redivac drain guides the stapler into the right position. The surgeon who performs the abdominal portion removes the drain and connects the anvil to the spindle. Firing of the stapler results in a “double pursestring – single stapled reanastomosis”.
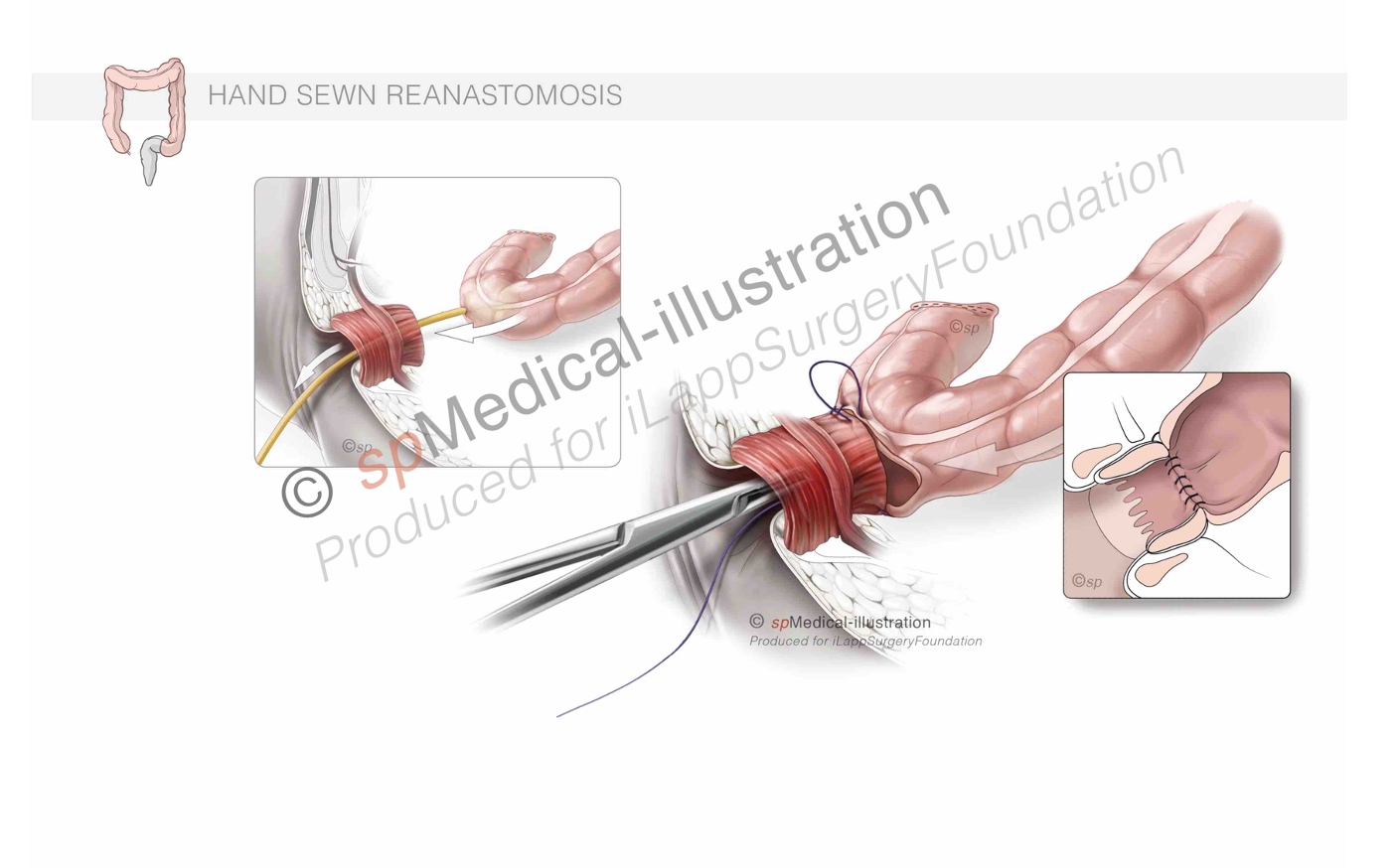
Hand-sewn coloanal anastomosis
In general a hand sewn anastomosis is performed when:
- a sleeve mucosectomy or intersphincteric resection is performed
- there is a risk of imbricating the vagina into the stapler
A traditional one-layer (or two-layer) anastomosis is created using interrupted polyglycolic acid 2-0 or 3-0.
A 14 Fr Foley catheter can be inserted into the proximal bowel to help deliver it through the anal canal.
When creating/fashioning a side-to-end anastomosis or J-pouch construction, an extra stitch on the side of the reservoir can help to orientate it and with the assistance of the laparoscopic surgeon a twist can be avoided. This can also be helpful for a stapled anastomosis.