Introduction to Major Hepatectomy
Edward Willems
Mathieu D’Hondt
Laparoscopic surgery was introduced over fifty years ago, and it has seen an increasingly rapid global uptake into several fields of abdominal surgery in the past decades.
The first case of a laparoscopic liver resection (LLR) was reported by Gagner and colleagues in 1992.(1) In the following years, there was a slow increase in the use of laparoscopy in liver surgery.
The first laparoscopic right hepatectomy (LRH) was reported by Huscher and colleagues in 1997.(2)
Several studies demonstrated the safety and feasibility of laparoscopy for minor liver surgery, and more and more surgeons started performing laparoscopic minor liver resections.(3-6)
Despite the efforts of these pioneers, the use of laparoscopy for major liver resections was still rare. The first series of more than 10 patients wasn’t published until 20047 and it wasn’t until the first consensus meeting on laparoscopic liver surgery in Louisville was held in 2008, that global diffusion of laparoscopic major liver resections started to expand.(8)
Several reasons can be defined for the slow uptake of laparoscopy for major liver resections.(9-13)
First, there is the risk of uncontrolled bleeding during hilar dissection or dissection at the hepatocaval confluence.
Second, laparoscopic mobilization of the heavy and fragile right hemiliver is difficult and also carries the risk of bleeding.
A third reason was the fear of gas embolism if vascular injuries occurred during a laparoscopic approach.
Another reason was the lack of appropriate instruments for transection of the bulky mass of liver parenchyma.
A last, important reason were oncological concerns regarding the safety of laparoscopic major liver resection with uncertainty regarding tumour margins.
Following the Louisville consensus meeting, several authors started reporting their experience with laparoscopic liver resections and laparoscopic major hepatectomies.(10-13-13-18) The Louisville consensus meeting was followed in 2014 by the second International Consensus Conference held in Morioka. The Morioka recommendations stated that laparoscopic major hepatectomies are still innovative procedures in the exploration fase, but that they are safe and feasible when performed by experienced surgeons. The need for formal education was also highlighted.(19-20)
Major hepatectomies are often considered as one entity in studies describing results and safety of laparoscopic and open liver surgery.
The important difference between a formal left and right hepatectomy was underlined for the first time during the Southampton Guidelines Meeting on Laparoscopic Liver Surgery in 2017 (21). The Southampton Guidelines state that a laparoscopic approach for right hepatectomy has several advantages compared to an open approach. There is less blood loss, lower morbidity and a shorter length of stay with no significant differences in operative time, blood transfusion rates and resection margins. The experts concluded that a laparoscopic right hemihepatectomy is safe and feasible in experienced hands.
In the beginning of laparoscopic liver surgery, no standardized techniques and procedures were available.
The first anatomical laparoscopic liver resection that became a standard procedure was a left lateral sectionectomy.(22)
For LRH, there was no standardized and reproducible technique available in the first years of laparoscopic liver surgery. Several pioneering surgeons developed their own technique for LRH.(7,16,23-24)
The importance of protocolization and simplification has been highlighted and some centers reported on their technique.(16,25-29) Different approaches have been described for a laparoscopic right hepatectomy, but none has been proven to be superior.
In the anterior approach, parenchymal transection is performed first, followed by ligation of the portal structures and division of the right hepatic vein.(25,27,30)
If the caudal or caudodorsal approach is used, parenchymal transection is performed after mobilisation of the right liver and ligation of the portal structures and sometimes even after dissection of the inferior vena cava and ligation of the right hepatic vein.(15-16,23,25,28)
The best approach depends on liver parenchyma, tumour size and location and the experience and preference of the surgical team. For large tumours however, the anterior should be preferred.(25)
Furthermore, the use of several technical tips and tricks have been discussed. Some authors prefer the use of a hanging maneuver (a tape slung around the liver in front of the IVC).(24,26)
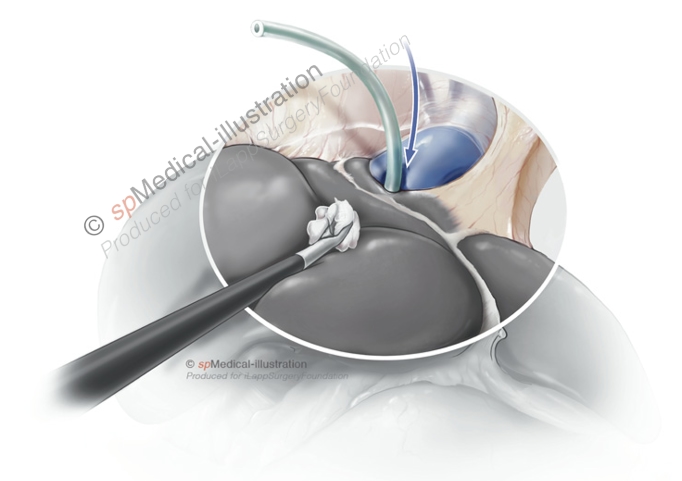
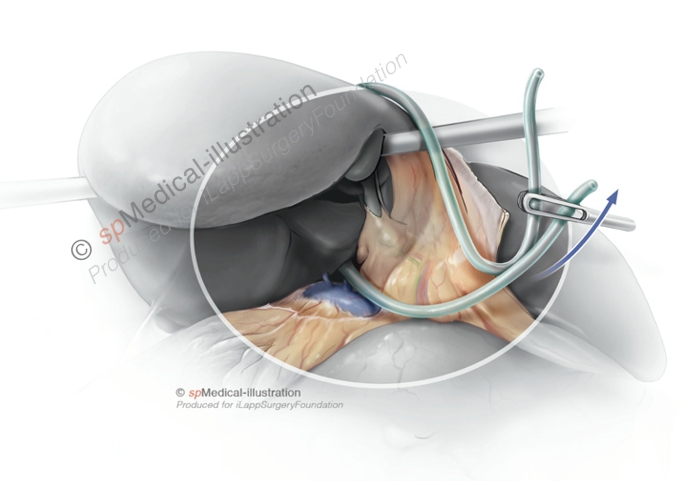
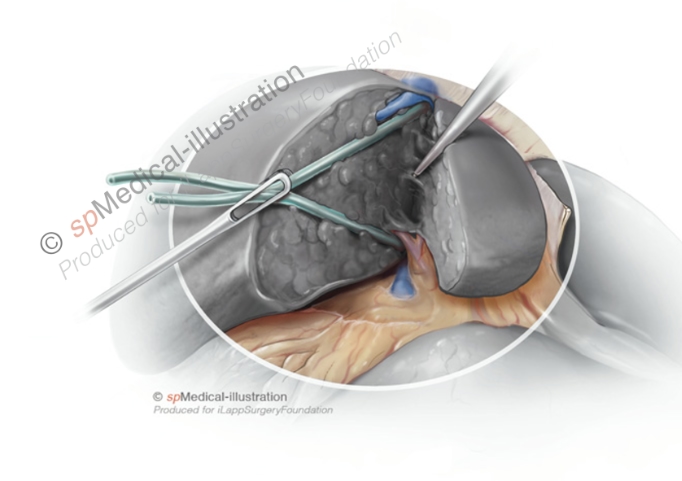
Laparoscopic Hanging Maneuver
Pringle maneuver is used by some authors, yet others prefer to perform hilar dissection and vascular control first.(16,30)
Others have suggested positioning the patient in left lateral or semiprone position to improve visualization and reduce the risks of haemorrhage.(26,29)
Independent of the technique, several authors reported on their results and the safety and feasibility of laparoscopic right hemihepatectomy.(16,23-24,26-29) Reports comparing the short-term outcomes of laparoscopic compared to open right hemihepatectomy have been published in the last few years.
Dagher et al found lower blood loss and shorter length of stay in the laparoscopy group, with similar complication rates and operative time.(12)
Abu Hilal and colleagues compared 36 laparoscopic with open right hepatectomies (ORH). They found longer operative times for LRH without significant differences in morbidity and mortality.(10)
Medbery et al found significant that operative duration, estimated blood loss, complications, length of stay and admission to ICU were significantly less in the LRH group.(15) In a cohort comparing LRH and ORH in patients with cirrhosis, Yoon and colleagues found no differences in complication rates, disease-free and overall survival.(30)
Since the majority of indications for liver resections are malignant diseases, concerns have been raised regarding the oncological safety of laparoscopy in liver surgery. These questions have been answered in several single and multicentre studies and the first randomised controlled trial (Oslo-Comet) was published recently. In this trial, long-term results for open and laparoscopic parenchyma-sparing liver resection for colorectal cancer metastases were not significantly different. The results of the first randomised controlled trial comparing laparoscopic and open major hepatectomies, the Orange-II Plus trial (Clinicaltrials.gov – Identifier: NCT01441856) are expected to be published in 2019. Some authors have reported their long term and oncological outcomes of laparoscopic major hepatectomy.(17,18) No significant differences in disease-free and overall survival have been found between laparoscopic and open major hepatectomy.